Efficient Appointment Booking with Real-Time Assistance
Patient Care
Reliable, Responsive, Around-the-Clock Patient Services
Boost patient satisfaction, enhance care quality, and reduce missed appointments with our always-available HelpDesk, trusted care, anytime.

Support Patients, Simplify Care
OACIS Health’s Patient Experience Management transforms healthcare by upgrading patient engagement at every touchpoint. From scheduling to patient support, around the clock, we ensure accessibility and patient satisfaction.
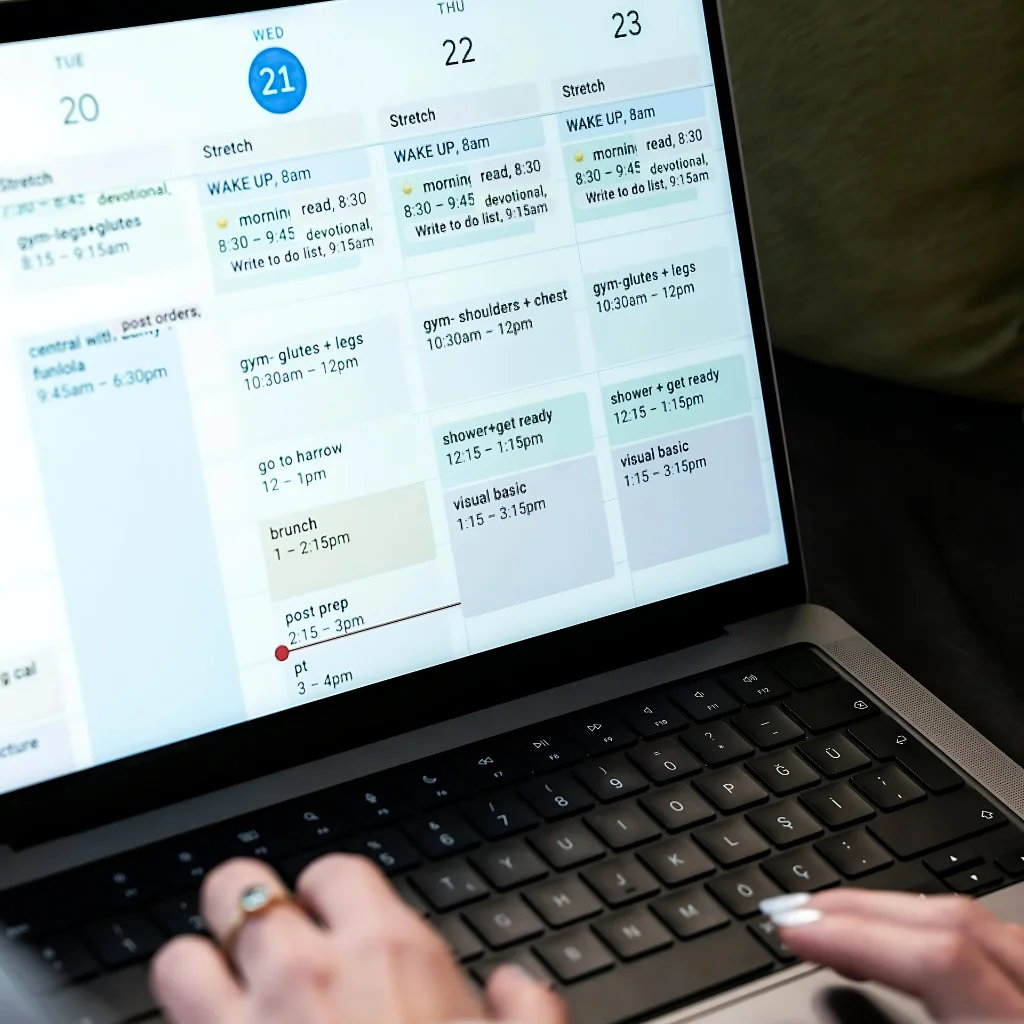
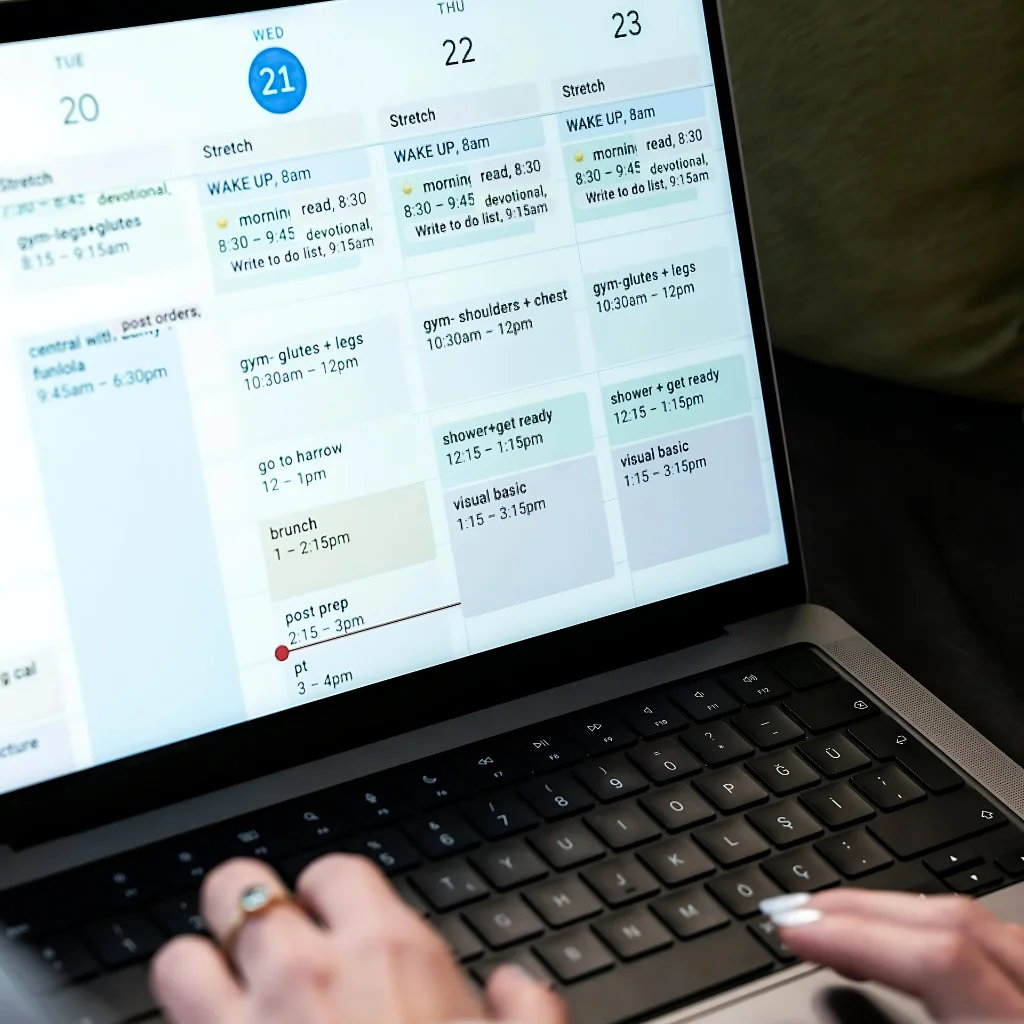
Patient Scheduling & Registration
Our easy-to-use system simplifies booking and lightens your team’s workload for a more efficient practice. Let patients schedule appointments whenever they want, from anywhere. With automated reminders and confirmations, our system helps reduce missed appointments, enhancing overall patient satisfaction and making scheduling as convenient as possible.

OACIS Health HelpDesk
Patient queries? No worries – our 24/7 HelpDesk is available at any moment to address all patient questions quickly and professionally. Whether it’s appointment scheduling, billing inquiries, or insurance-related concerns, our trained agents ensure every patient receives accurate information and a positive experience—helping your practice build trust, reduce administrative burden, and improve overall satisfaction.
Testimonials
Hear From Our Esteemed Clients
Real stories from healthcare providers who trust OACIS Health to streamline their revenue cycle and improve patient care.
Our denial rate was almost 20% before transitioning. This team implemented clear billing workflows and payer-specific strategies, reducing denials to under 5% and improved our first-pass claim acceptance rate to over 98%. Collections rose by 22% in the first quarter, and our bad debt was reduced to near zero. Their performance exceeded all expectations.
This team brought clarity and control to our pediatric billing processes. They introduced a structured guideline system that brought down claim rejections from 12% to under 3%, while denial rates dropped by 40% within 60 days. Clean claim submission is consistently above 97%, and our AR over 90 days was cut in half. Their attention to detail is phenomenal.
Our internal medicine practice saw a measurable improvement in billing KPIs after switching. Aging over 90 days dropped from 28% to under 10%, and our net collection rate increased to 98%. Denials decreased by 35%, and we now receive most payments within 25 days of submission. Their performance-driven model helped stabilize and grow our revenue.
Working with non-par insurance plans has always been a pain point due to low reimbursements and complex negotiation processes. This billing team brought in a dedicated strategy for timely filing and payer negotiation support, which resulted in over 30% improvement in our payment for non-par claims. Our previously written-off claims were recovered with professional handling. Their experience with out-of-network billing made a significant financial difference.
Let's Modernize Your Patient Experience
Ready to Deliver 24/7 Access Without the Overhead? Partner with us for smarter scheduling, better support, and happier patients.
